Dear Reader,
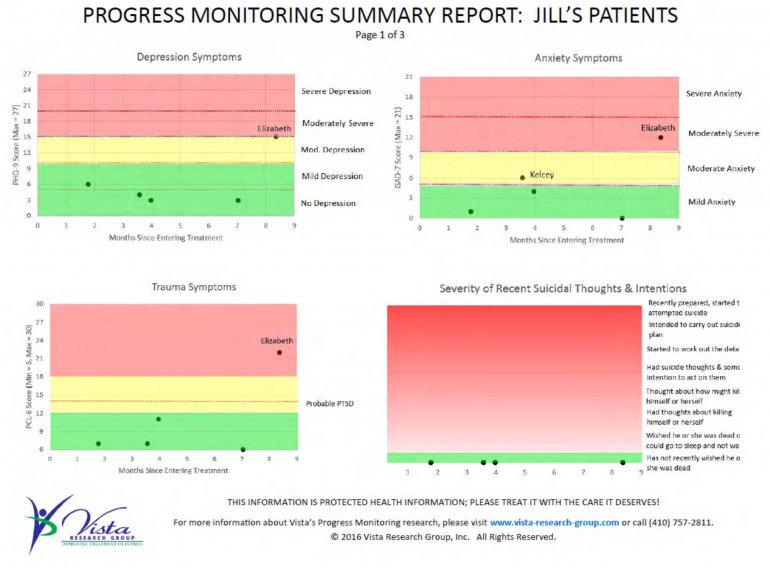
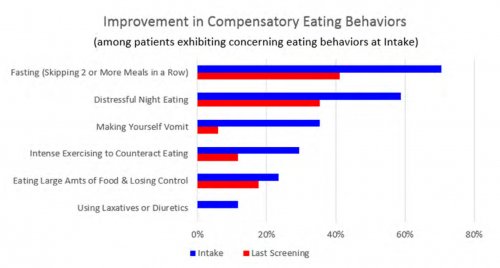
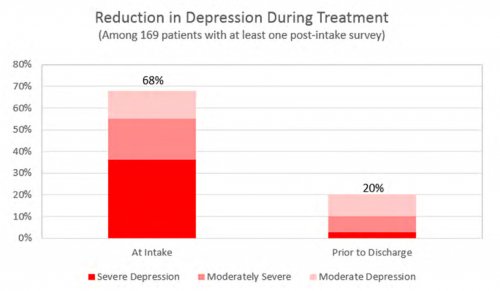
Research has shown that regularly providing clinicians with data about how their patients are feeling helps patients get better faster regardless of the type of therapeutic approach being provided. As a result, interest in using patient-reported results to improve substance use disorder and behavioral health treatment results has been growing rapidly.
But until recently, there haven’t been tools that help centers easily monitor how their patients are doing either during or after treatment. Vista Research Group launched INSIGHT Addiction™, INSIGHT Behavioral™ and RECOVERY 20/20™ to enable programs to effortlessly collect and analyze patients’ outcome measures to enhance the treatment they’re providing.
This eBook summarizes what we’ve learned from our clients and their patients about how clinicians can use outcome measures to help patients get better faster. We also recommend how your management team can use the tremendous insights provided by this type of research to improve your program’s treatment outcomes and bottom line.
If you like Vista’s approach, the final two chapters explain how you can get started using our software to view patient outcome measures today. Alternatively, you can use the principles and examples in this eBook with other measurement-based care options or by building your own tools. Please join me on an exciting journey into the rapidly-emerging world of using outcome measures to provide better care to patients suffering from addiction and other behavioral health disorders. Hang on tight!
Joanna Conti, Founder & CEO
Vista Research Group, Inc.
September 2017