At the request of one of our clients, we made what I considered a minor change to our intake questionnaire recently and learned something quite interesting.
We previously asked patients a screening question to determine whether another issue—such as a personality disorder or gambling addiction—had been a significant factor in their decision to start treatment. Unless a patient answered “yes,” we wouldn’t inquire further about ADHD. Using this approach, fewer than 2% of adult SUD patients in the Vista Research Network reported that Attention-Deficit/Hyperactivity Disorder (ADHD) had contributed to their needing treatment.
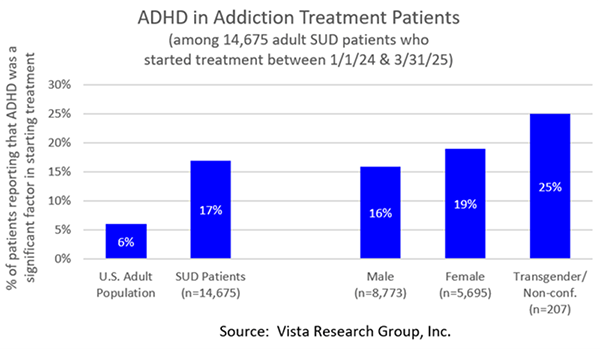
However, when we combined the two questions and listed ADHD as a possible issue up front, suddenly 17% of all adult SUD patients reported that ADHD had been a significant factor in their starting treatment. This is almost three times higher than the CDC’s estimate that 6% of American adults have ADHD!
Interestingly, 19% of women in treatment reported that ADHD had been a factor compared to 16% of men. And while it’s a very small base, 25% of transgender/non-conforming patients reported that ADHD had played a role in their needing treatment.
Why People with ADHD Are Prone to Addiction
Research shows that many people with ADHD have genetic variants that reduce dopamine activity in areas of the brain involved in attention, motivation, and impulse control. Some individuals turn to substances like stimulants or alcohol in an effort to self-medicate and temporarily boost their dopamine levels.
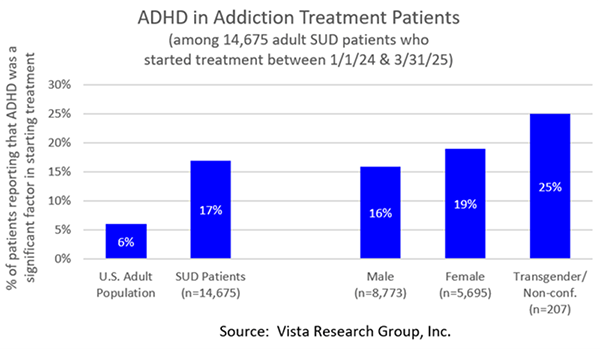
Vista’s research bears this out. Twenty-three percent (23%) of patients with ADHD name a stimulant as their primary drug of choice compared to only 19% of non-ADHD patients:
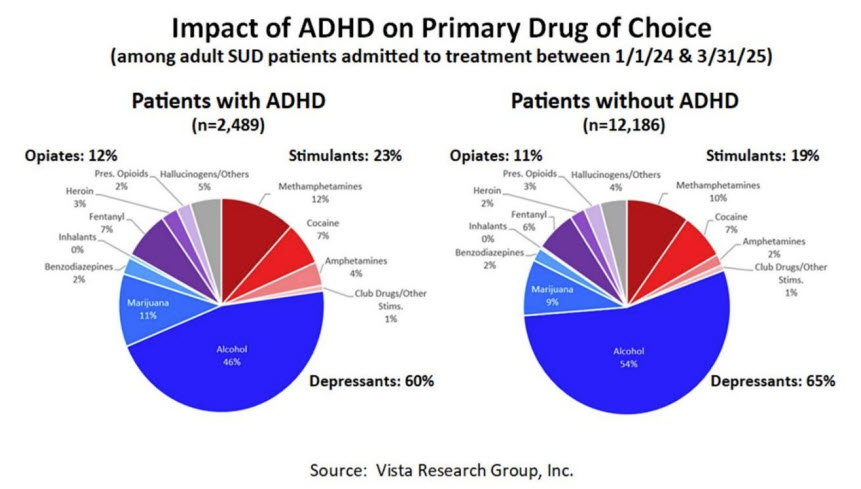
Additionally, among patients in treatment for Alcohol Use Disorder, those with ADHD report drinking more drinks per day that those who don’t have it:
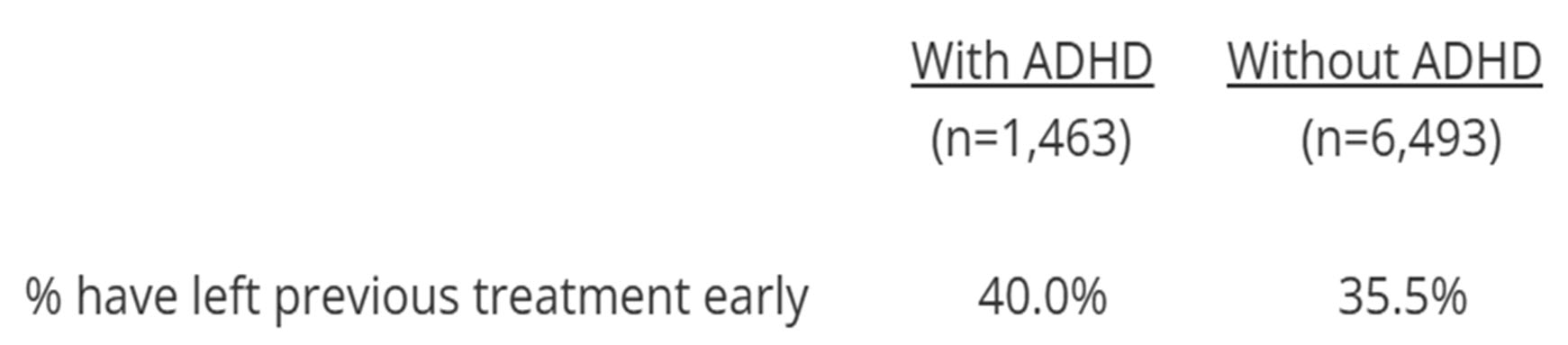
A second common characteristic of individuals with ADHD is impulsivity. Not surprisingly, they are more likely than patients without ADHD to have left a previous treatment episode without completing all recommended treatment, such as by leaving against medical advice or being asked to leave:
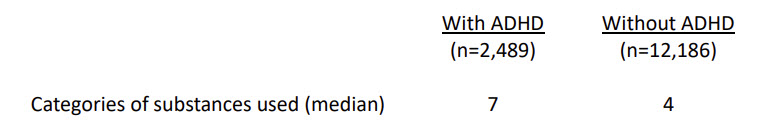
Patients with ADHD are also more likely to have used more different types of drugs than non-ADHD patients. Of the 15 categories of substances Vista asks about (alcohol, marijuana, amphetamines, cocaine, methamphetamines, prescription opioids, heroin, fentanyl & other synthetic opioids, benzodiazepines, stimulants, inhalants, club drugs, tranquilizers, hallucinogens, and other drugs), the patients with ADHD report having used substances in 7 categories compared to only 4 for patients without ADHD:
Why ADHD Makes Addiction Harder to Treat
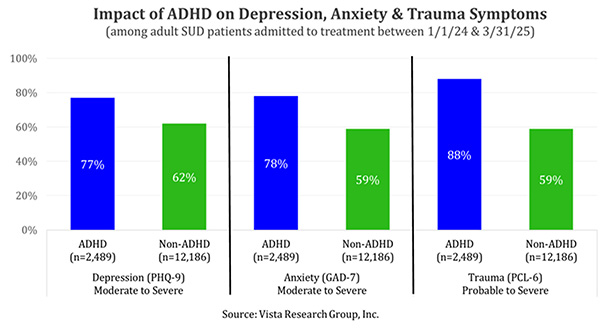
More severe co-occurring disorders: On average, more ADHD patients report experiencing moderate to severe symptoms of most co-occurring disorders in the 30 days prior to treatment than those without ADHD. This difference is particularly stark with depression, anxiety & PTSD symptoms:
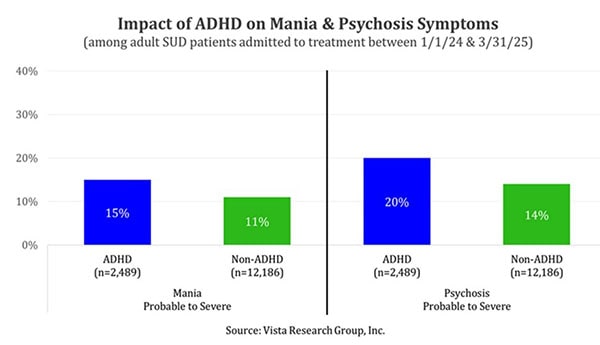
More ADHD patients also report having probable to severe symptoms of mania and psychosis than non-ADHD patients:
Greater likelihood to leave treatment early: A second challenge of treating SUD patients with ADHD is that their impulsivity and potentially aggressive behavior make it somewhat more likely they won’t complete all recommended treatment:
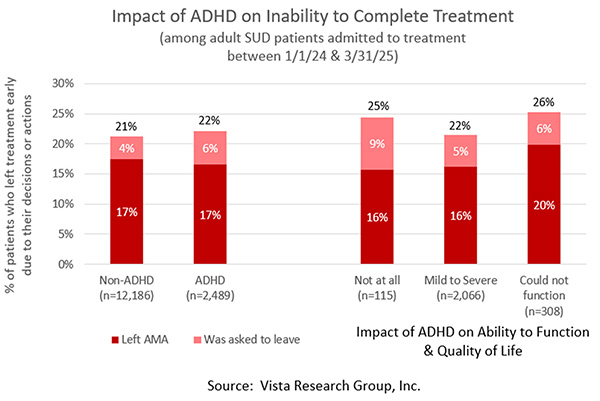
It’s particularly interesting to see how the answer a patient gave to the following question affected their ability to complete treatment:
“In the month before you began treatment, how much did your ADHD
affect your ability to function normally as well as your quality of life?”
Patients who answered “to the point I could not function” were more likely to leave against medical advice. Patients who answered “not at all” were more likely to be asked to leave. Patients who answered “mildly”, “moderately” or “severely” (and, perhaps, had a better understanding of how to manage their ADHD), were almost as likely to complete treatment as those without ADHD.
ADHD Patients Are Less Likely to Recover
Following SUD Treatment
All of these factors combine to make it more difficult for individuals with ADHD to recover from addiction. Among adult SUD patients who were in treatment after January 1, 2024, only 35% of patients with ADHD were reachable and abstinent for at least the last 30 days at six months post-treatment. This is substantially less than the 41% of non-ADHD patients who reported being abstinent at this point:
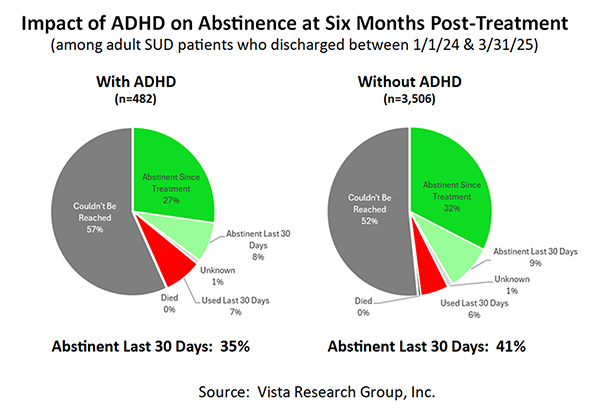
As this data makes clear, ADHD is more than just a co-occurring diagnosis—it’s a meaningful driver of treatment complexity, early dropout, and lower recovery rates. For clinicians, recognizing and actively addressing ADHD symptoms in addiction treatment isn’t optional; it’s essential to improving outcomes. The better we understand the interplay between these conditions, the more effectively we can help our patients achieve long-term recovery.



