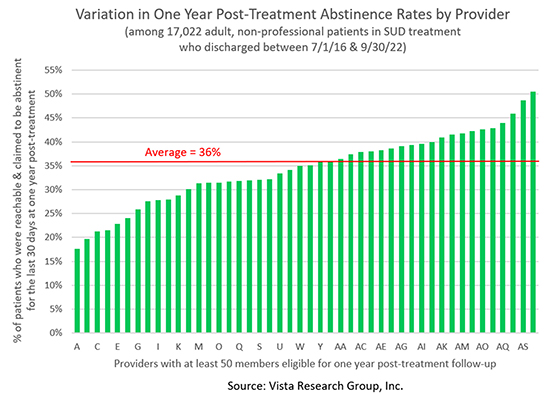
We’ve known for years that the likelihood an individual struggling with addiction will be meeting their drug and alcohol usage goals one year after treatment varies tremendously by the treatment center they attended:
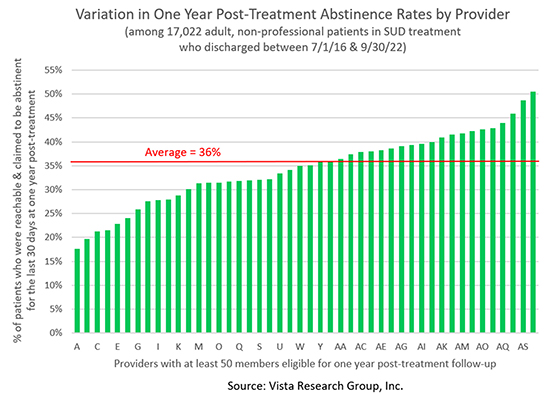
I was surprised, however, to discover that the graph of patient outcomes by health insurance payer looks almost identical:
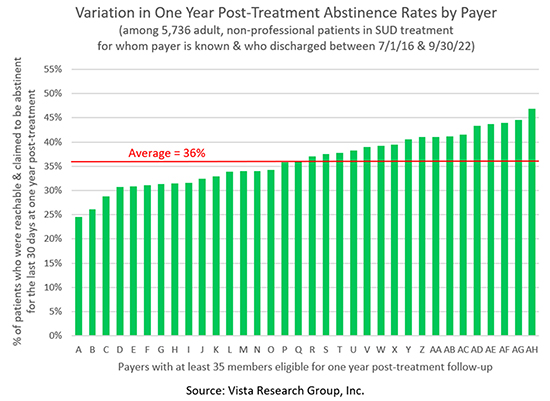
Close to half (47%) of the members of the health insurance company with the best outcomes reported successfully abstaining from alcohol and non-prescribed drugs for at least the last 30 days one year after treatment. At the other end of the spectrum, less than one-quarter (24%) of the members of the health insurance company with the worst outcomes reported similar success.
Wow! Are you as surprised by this as I am?
What Accounts for This Variation in Payer Outcomes?
Short treatment stays clearly account for the poor results of some of the payers. Several of the payers with the poorest outcomes have median treatment stays of only 20 to 22 days, while none of the payers with above-average outcomes have median treatment stays anywhere near this short.
Another factor that clearly impacts outcomes is the strength of the provider network the payer is using. Not surprisingly, the payers with better outcomes are sending more of their patients to 5-star treatment centers – those in which at least 40% of their patients are in recovery one year later – than those with poorer outcomes.
These factors don’t begin to account for all of the differences. But rather than spend our time trying to tease out all the correlations, we should focus on developing a case to convince payers that paying for higher-quality treatment will save them money.
Convincing Payers to Invest in Higher-Quality Treatment
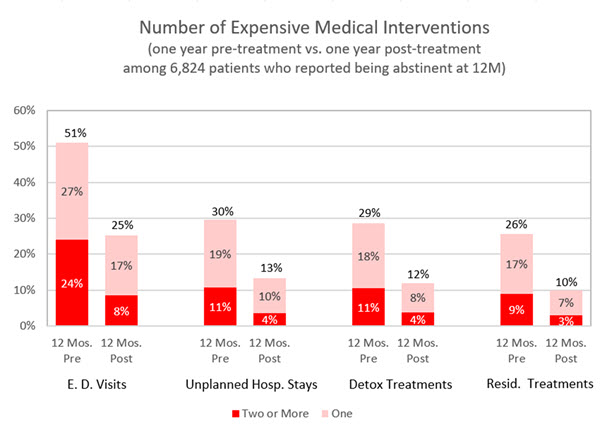
Vista’s research clearly shows that patients who are abstaining from alcohol and non-prescribed drugs for at least the last 30 days one year after discharge have far fewer expensive emergency department visits, unplanned hospital stays, and detox and residential treatments in their post-treatment year than would be predicted by their pre-treatment year:
But showing payers Vista’s patient-reported data is probably not going to get them to change their belief system. To convince payers that they’ll save money by investing in more effective treatment, we need to work with the claims data they know and trust. So the Conquer Addiction Research Institute, part of the nonprofit my daughter and I started to help more people recover from addiction, is raising $250,000 to purchase and analyze claims data for 508,000 individuals in SUD treatment between January 1, 2018 and December 31, 2021. The objective of the study is:
To identify actions payers can take that will simultaneously help more members recover from addiction while saving money
By comparing total medical and pharmaceutical spending in the year prior to treatment to spending in the post-treatment year, we expect to be able to show that paying for effective treatment saves health insurance companies money in the short-term. We’ll even be able to analyze the impact of ten factors Vista has shown improve treatment outcomes by inserting patient data for 6,657 Vista patients into de-identified claims datasets.
This Payer Project is Phase One of a much bigger research project we hope will help millions more people recover from addiction by 2030. If you’re interested in working with a small group of treatment center leaders to support these exciting projects, please reach out to info@vista-research-group.net and say “I’m in.”
Joanna
P.S. While we’re on the subject of working with payers, I have a request. As payroll costs skyrocket and reimbursement rates don’t, I’m getting increasingly concerned about the ability of treatment centers to continue to provide effective treatment. Could you take a few minutes now to answer several questions about how your treatment center has been impacted by these issues?
State of Addiction Treatment 2023 Questionnaire
Completing the survey shouldn’t take you more than three minutes, I promise! Your answers will be kept strictly confidential, but we’ll share our overall findings publicly and with everyone who participates. Thank you for your support!

