Treating addiction is incredibly difficult. Our research shows that despite the best efforts of their therapists, many (if not most) patients struggle to achieve lasting recovery.
Research shows that regularly providing clinicians with data about how your patients are feeling helps your patients get better faster regardless of the type of therapeutic approach being provided. Measurement-based care (MBC) makes a big difference. MBC uses real time data to track patient progress, identify issues early, and adjust treatment plans to better suit each patient’s needs. This approach helps treatment centers offer more effective and responsive care, leading to better and more lasting recovery for patients.
Understanding What Measurement-Based Care Is (and What Is Not)
What is MBC?
Measurement-based care, or MBC, is the evidence-based practice of using data to guide treatment decisions.
In simple terms, it means keeping tabs on a client’s progress throughout treatment. MBC lets clinicians and clients regularly connect, review symptom changes together, and uncover insights that help shape clinical decisions. The ultimate goal of MBC is to gather enough meaningful data to tailor treatments and interventions to the individual needs of each client.
MBC goes by a lot of different names. You might hear it referred to as Progress Monitoring, Outcomes Measures, Routine Outcome Monitoring, or Patient Reported Outcome Measures (PROMs), or Feedback-Informed Treatment. Whatever the name, the idea is the same: leveraging patient data and insights to collaborate on treatment decisions, increase client engagement, and, ultimately, improve treatment outcomes.
What MBC is all about:
- Continuous Tracking: Conducting regular check-ins to monitor a patient’s mental and emotional health.
- Objective Data: Using structured assessments to collect reliable, unbiased PROMs.
- Patient Engagement: MBC relies on clients actively participating by giving feedback on their symptoms and progress.
- Making Informed Decisions: Clinicians use the data to measure and track patient improvement over time.
What MBC is not:
- One-Time Assessments: MBC isn’t a single data point. For MBC to work, organizations must consistently collect data throughout treatment.
- Subjective Impressions: While clinician observations matter, MBC requires structured, validated patient-reported assessments for objective data.
- Static Treatment Plans: With MBC, treatment plans should evolve based on data, not stay fixed.
Post-Treatment Outcomes: MBC focuses on real time data during treatment, not outcomes after treatment ends. Read more about the importance of measuring post-treatment outcomes and how do so here.
Until recently, many organizations lacked the tools to easily monitor patient progress during and after treatment. This made it difficult for treatment centers to keep track of client progress, identify emerging issues early, and make timely adjustments to treatment plans.
But research indicates that leveraging data and insights, both during and after treatment, can be incredibly effective at helping patients get better faster. For example, Dr. Ingrid Carlier’s meta-analysis of 45 mental health-related clinical trials showed that patients whose clinicians had access to measurement-based care got better faster in 65% of the cases, including all three of the clinical trials conducted during addiction treatment.
This is Where Vista Research Group is Changing the Game
Here at Vista, we use a number of personalized assessment tools to capture real time behavioral measures on disorders like anxiety, depression as well as how patients feel overall. Our trailblazing measurement-based care software allows clinicians to quickly identify and treat co-occurring disorders, spot patients who aren’t progressing as expected, and flag patients who are at risk of leaving treatment against medical advice.
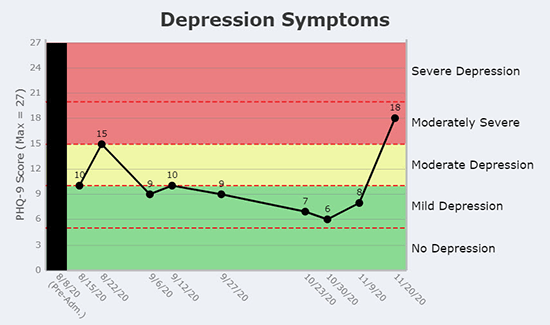
With Vista’s platform, patient’s self-reported feelings, concerns, and thoughts about the treatment are instantly presented in color-coded, easy-to-understand graphs that make it clear how a patient is doing:
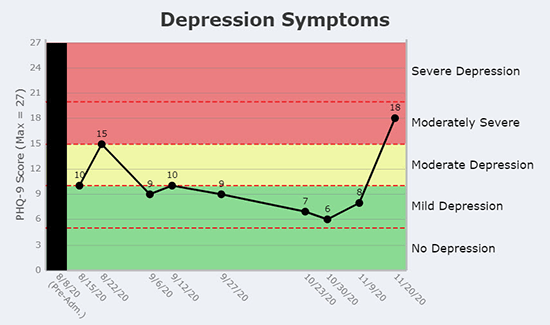
The patient above reported being severely depressed in the 30 days before they started treatment. Fortunately, their depression symptoms lessened over the time they were in treatment. However, something has just caused this patient’s depression symptoms to spike.
Why Treating Mental Health Issues During Addiction Treatment Matters
Addiction and mental health disorders often overlap. It’s common for someone struggling with addiction to also have conditions like depression, anxiety, or PTSD. Ignoring these issues can make recovery much harder.
Treating mental health issues during addiction treatment is crucial because these conditions often fuel each other. For example, untreated depression can lead to increased substance use as a coping mechanism, while addiction can worsen mental health symptoms.
The good news is that if a patient’s depressive symptoms can be alleviated, their likelihood of achieving long-term sobriety improves. In a study looking at 298 American male veterans completing a 21-day residential treatment, results showed that patients who were depressed at admission but not three months after treatment had even better recovery outcomes than those who were never depressed.
How Vista Helps
MBC allows clinicians to monitor both addiction and mental health symptoms in real time, which translates into quicker interventions and more personalized modifications to the treatment plan. For example, if a patient’s anxiety spikes, the treatment team can add targeted therapies or adjust medications right away.
Vista’s tools are designed to track a wide range of mental health conditions. But instead of arbitrarily choosing which co-occurring disorders to monitor each patient for, Vista’s INSIGHT Addiction™ uses academically validated screening questions to identify the ones each patient is likely to be struggling with. If a patient doesn’t answer any of the screening questions positively for a disorder, Vista doesn’t frustrate the patient by making them complete an assessment for a condition they’re unlikely to have.
What’s also great about this approach is that it lets the patient identify for themselves how they’re feeling. Users of Vista’s software have found that a significant number of their patients are dealing with unsuspected co-occurring disorders. This insight allows for more accurate and personalized treatment plans, ultimately improving patient outcomes.
The Benefits of Measurement-Based Care in Addiction Treatment
Throughout our 9 years of experience monitoring over 90,000 patients, we’ve seen firsthand how MBC can boost patient outcomes and help organizations operate more efficiently. Here are some key benefits of MBC for both patients and treatment centers:
Benefits of MBC for Patients
Faster Improvement
MBC helps patients get better faster. Dr. Ingrid Carlier’s 2012 meta-analysis of 45 mental health-related clinical trials found that progress monitoring sped up recovery 65% of the time, including in all three of the trials at addiction treatment facilities. The key is tracking how patients are feeling throughout their treatment and reporting this information to clinicians in a way that’s easy to understand and act upon.
Here at Vista, we’ve seen firsthand how progress monitoring can accelerate recovery for several reasons. For one, it enables the early identification and treatment of co-occurring disorders, which have often contributed to the patient’s addiction. Additionally, progress monitoring makes it clear when a patient isn’t improving as expected, so clinicians can adjust the treatment plan early in the treatment process.
Personalized Treatment Plans
Measurement-based care (MBC) takes treatment plans to a whole new level of personalization, making sure they really fit each patient’s unique needs. In the past, addiction treatment often relied on one-size-fits-all approaches that didn’t take into account the individual differences in patient experiences, symptoms, strengths, and preferences. But MBC changes that by continuously gathering data on various aspects of a patient’s condition through standardized assessments and other measurement-based care questions.
One of the most important things in effective addiction treatment is understanding a patient’s strengths right from the start. And sure, assessments help identify symptoms, but knowing a patient’s strengths and what they value right from the beginning is just as crucial. For example, if someone with a history of trauma has been using alcohol to cope, simply taking the alcohol away isn’t enough—you need to help them find healthier ways to deal with their PTSD symptoms. Recognizing a patient’s strengths allows you to build on them and replace harmful behaviors with positive ones that align with their abilities. As you keep gathering data, you’re not only tracking how their symptoms improve but also how they’re growing in their ability to handle life’s challenges.
Enhanced Patient Engagement and Empowerment
Getting patients actively involved is crucial for successful addiction treatment, and MBC really helps with that by putting patients right in the middle of their own recovery process. When patients regularly report their symptoms and progress through surveys and assessments, they feel more connected and invested in their journey. This sense of involvement and ownership can make a big difference in how committed they are to sticking with their treatment plan.
Plus, evidence suggests that patients who feel empowered are more likely to follow through with their treatment, show up for therapy sessions, and stay engaged in their recovery. For example, if a patient regularly tracks their mood and cravings through an MBC platform, they can become more aware of their triggers and how far they’ve come. This awareness can be a strong motivator, helping them stay on track with their treatment and actively working toward their recovery goals.
Early Identification of Issues
One of the biggest perks of MBC is how it helps catch potential problems early, so they don’t turn into bigger setbacks. Regular assessments and feedback give clinicians a real time view of what’s going on with a patient, allowing them to spot early warning signs of relapse, emerging mental health issues, and other complications before they spiral out of control.
Sometimes, when patients first come in, they don’t have the words to describe what they’re feeling or what they’re going through. This is where MBC assessments really shine, since they are designed to ask patients about their symptoms in words they understand. Once patients have described their experiences and behaviors, clinicians can build on that information to tailor their treatment plan effectively.
Additionally, if a patient reports feeling more stressed or having stronger cravings during their weekly check-in, the clinician can step in right away to adjust the plan. This might mean adding extra support sessions, tweaking medication, or introducing stress management techniques. Taking action quickly like this can make all the difference in preventing relapse and keeping the patient on track with their recovery goals.
Better Mental Health Management
MBC gives us a clear and structured way to keep an eye on mental health issues that often co-occur with substance use disorders. With regular assessments, we can track changes in mood, anxiety, and other mental health factors, making it easier to tackle both addiction and mental health needs at the same time.
Take a patient dealing with both depression and substance use disorder, for example. With MBC, their depression symptoms are regularly monitored right alongside their addiction treatment. If their depression starts to worsen, the treatment team can step in and adjust the plan. By treating all of the patients’ issues, we can ensure the patient gets the comprehensive care they need.
Strengthened Therapeutic Alliance
Building a solid connection between a patient and their therapist is crucial for successful addiction treatment, and MBC helps make that happen. By regularly gathering data and having feedback sessions, MBC shows patients that their opinions and experiences matter, which boosts trust and collaboration between client and therapist.
For example, when therapists regularly check in on patient-reported outcomes and talk about them during sessions, they get a clearer picture of what the patient is going through, both in and out of therapy. This helps patients open up about their struggles, leading to more effective treatment.
While you’re asking patients about their symptoms, it’s also wise to gauge how they’re feeling about working with their therapist. Each Vista survey includes questions about how the patient rates their relationship with their therapist and how helpful recent therapy sessions have been in meeting the patient’s treatment goals.
Benefits of MBC for Treatment Centers
Improved Treatment Outcomes
The biggest benefit of measurement-based care in mental health and substance use treatment centers is better recovery outcomes. When you use data to guide treatment, success rates go up, leading to more patients achieving long-term recovery. These successful outcomes not only boost the center’s reputation but also build trust and attract more patients.
Enhanced Operational Efficiency
MBC can help streamline the day-to-day operations in treatment centers. Using standardized assessments cuts down the time providers spend on evaluations, so they can focus more on actually caring for patients. Plus, automated data collection and analysis tools can reduce the admin work and free up more resources for patient care.
With Vista’s MBC tools, treatment centers can sync up MBC software with their existing electronic health records (EHR) systems. Knowing that the results of their patients’ assessments will be immediately uploaded to their medical record allows clinicians to focus on interacting with patients and planning their treatment.
Additionally, Vista’s clinical users regularly report that their sessions are much more productive when they can see updated information about how their patients are feeling before the session starts. Having this information in advance allows the clinician to dive immediately into a useful discussion about the patient’s current challenges.
Financial Benefits
Implementing MBC can give a big boost to the financial health of your treatment centers in several ways. Insurance companies are increasingly looking for evidence-based practices when setting reimbursement rates, and MBC provides the hard data that proves treatment effectiveness.
On top of that, the ongoing data from MBC can make it easier to get more days of treatment approved by insurance providers. For example, UR teams can use the fact that a patient is still feeling moderately depressed to argue against stepping the patient down to a lower level of care.
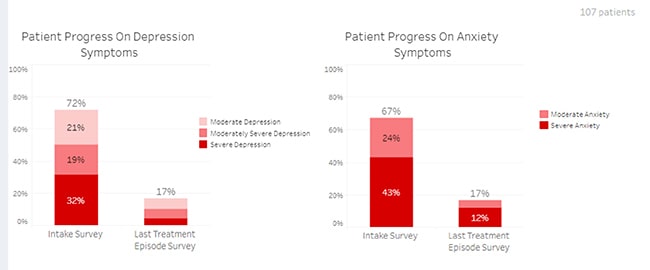
Additionally, your measurement-based care results can be very helpful in negotiating higher reimbursement rates with your payers. For example, payers will be very interested in seeing how the severity of their members’ co-occurring disorders decreased during treatment:
Continuous Improvement
MBC gives treatment centers a wealth of data to dig into, helping you spot trends and patterns in how well patients with different treatments or at different locations are doing. For example, a center might find that a specific therapeutic approach works better for a specific demographic, or even pinpoint if a particular patient is not happy with the treatment they’re getting and redirect more time and/or resources to support them, helping ensure they stay engaged and complete their treatment successfully.
Plus, regularly reviewing MBC data can highlight where staff might need extra training or support. If some therapists consistently get better results, you can look into what they’re doing right and share those techniques with the rest of the team. Conversely, if the data shows gaps in certain areas, you can create targeted training programs to help address those gaps and improve overall care.
How to Set Your Treatment Center Up for Success with MBC
Bringing measurement-based care into your mental health and substance use treatment can make a huge difference in patient outcomes, streamline operations, and even boost financial stability. But there are a lot of factors to take into consideration to ensure your center implements MBC effectively. In this last section, we discuss some of the key decisions you need to make, and how Vista’s cutting-edge software, analytical tools, and expert guidance can help your center (almost) effortlessly transition to MBC:
Choose Assessments That Are Meaningful and Relevant for the Patients You’re Treating
It’s crucial to use assessments that are meaningful and relevant to the patients you’re treating. This means opting for academically validated measures that are designed for self-reporting, so patients can easily fill them out themselves. These tools should be sensitive to changes in a patient’s condition and reasonably quick to complete, so they don’t feel like a burden.
Vista offers a suite of validated, reliable tools tailored for addiction treatment that can be seamlessly integrated into your center’s workflow to ensure data collection is efficient, relevant, and effective.
Minimize the Time It Takes Your Staff to Collect and Process Patient Data
Let’s face it—everyone’s busy, and if gathering, analyzing, and sharing patient data with your clinicians is going to take hours every week, it’s probably not going to consistently happen. The more time-consuming it is, the more likely it is to fall by the wayside.
To keep MBC running smoothly, it’s important to streamline the process as much as possible. We recommend investing in tools that automate data collection and analysis, so your team can focus on what they do best—caring for patients. Make sure the data is available to your clinicians when they need it without adding extra work or stress to anyone’s plate.
Make It Easy for Your Clinicians to Access and Understand Your Patient Feedback
For your clinicians to really benefit from patient feedback through MBC, it has to be easy to access and simple to understand. Make sure the data is available in real time and laid out in clear, straightforward graphs. This way, your team can quickly see what’s going on without wading through all sorts of complicated details.
Also, set up alerts for red flags, such as patients reporting dangerous thoughts or behaviors, so clinicians can respond right away. Giving them access to detailed responses and using open-ended questions helps them get a fuller picture of what the patient is experiencing. The easier it is for your team to access and make sense of this feedback, the better they can support their patients.
Fostering a Culture of Data-Driven Care
Building a culture that values data-driven decision-making is the key to getting the most out of MBC quickly and effectively. Make it a habit to review data regularly, talk about the findings in team meetings, and use that info to guide clinical decisions. At Vista Research Group, we can help make this happen by offering ongoing support and resources to seamlessly weave MBC into your center’s everyday practices.
Engaging Patients in the Process
One of the most important parts of MBC is getting patients actively involved in the process. This means explaining why regular assessments are important, encouraging them to be honest and detailed in their reporting, and having open conversations about any treatment adjustments based on the data. Vista Research Group’s tools make this easy with user-friendly patient interfaces that help keep them engaged and ensure accurate data collection.
Compare Your Aggregated Results to Benchmarks to Identify Opportunities to Improve
Taking a step back to review your aggregated results against industry benchmarks can help highlight areas where your treatment center can improve. Seeing how you measure up against the broader field helps you identify both strengths to build on and areas that need attention.
With those insights, you can make targeted changes that lead to better outcomes for your patients. Use that big-picture view to keep your center moving forward and continually improving.
Review Patient Assessment Data In Your Clinical Staff Meetings
Bringing patient assessment data into your clinical staff meetings reaps tremendous benefits. In the early days, there will usually be a few clinicians who are reluctant to start using patient data to inform care. If they know they may be asked about their patients’ assessments at the staff meeting, they’ll at least start reviewing their patient data prior to the meeting. As other clinicians start sharing something surprising they learned or a treatment plan change they made as a result of their patients’ MBC feedback, these clinicians will almost always join the bandwagon.
Additionally, as the clinical team spends time together reviewing patient data, clinicians will share insights and ideas that could result in treatment breakthroughs. The resulting collaboration can have a big impact on how well your team supports patients through their recovery.
Make Sure to Act on the Patient Feedback You Receive
Ultimately, gathering patient feedback is only half the battle—what really matters is what you do with it. Use this feedback to identify patients who aren’t progressing well, act on any unexpected findings, and keep an eye out for signals of a potential relapse.
Taking the time to review and act on this feedback shows your patients that their input truly matters and helps you make meaningful improvements to their care. Whether it’s adjusting treatment plans, improving communication, or addressing specific concerns, acting on feedback not only boosts patient satisfaction but also strengthens trust and engagement. Turning insights into action will help more of your patients recover from addiction.