Based on the many discussions I’ve had with treatment center leaders over the years, I suspect that negotiating with health insurance payers for a fair reimbursement rate is one of (if not the most) challenging aspects of running a treatment center. And it seems to be getting even harder.
To help our clients prepare for these make-or-break negotiations, Vista produces annual Payer Summary reports at no additional charge for full members of the Vista Research Network. These reports focus on the types of data of most concern to health insurance payers.
Financial Metrics
Providers and payers look at patients through a different lens. Since payers are heavily focused on minimizing cost, probably the most important metric you can show them is how much they saved in medical spending for their members in the post-treatment year compared to what they were spending the year prior to treatment.
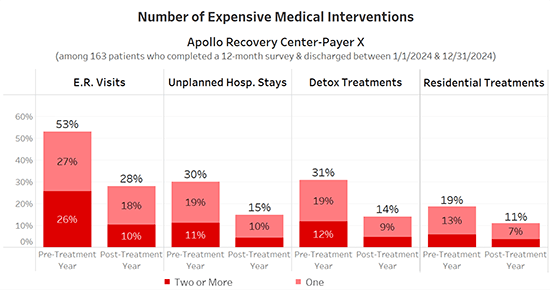
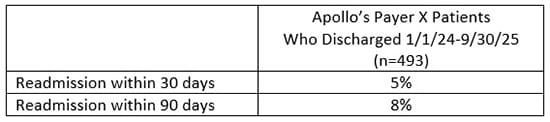
Vista’s research shows that patients completing 12 month post-treatment outcomes surveys average only about half as many emergency department visits, unplanned hospitalization stays and detox treatments in the year after they leave treatment compared to their pre-treatment year:
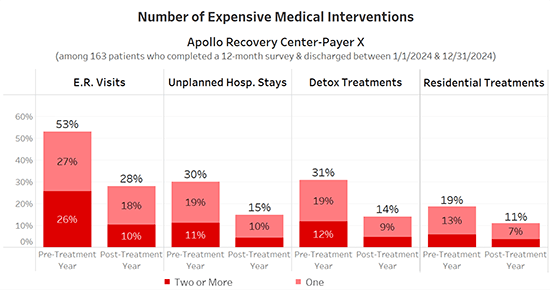
We take this one step further, and estimate the amount of money the payer saved in the post-treatment year for these members based upon the average cost for SUD-related interventions in that region of the country:
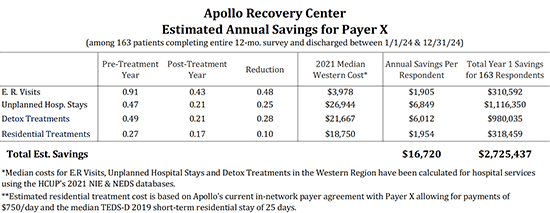
Another financial metric of key concern to payers is the center’s 30- and 90-day readmission rates:
Treatment Effectiveness Data
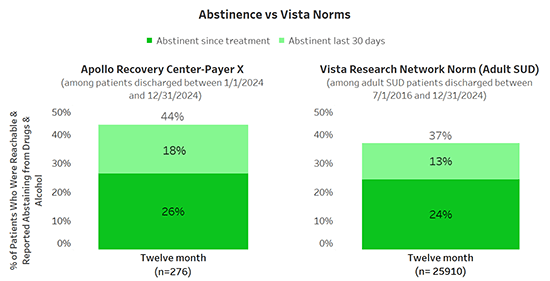
Vista also includes the most compelling patient-reported treatment effectiveness data in your Payer Summary Report. We’ll show that substantially more of your patients are meeting their drug and alcohol usage goals one year after discharge compared to Vista’s norm:
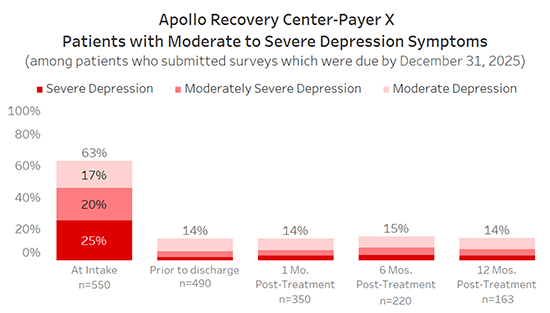
Payers should also be impressed to see that the severity of your patients’ co-occurring symptoms drop dramatically during treatment and remain low throughout the post-treatment year:
The Payer Summary Report also includes treatment completion data, patient satisfaction scores, improvement in quality of life measures such as stable housing, and two HEDIS Measures (access to care and depression remission or response) of importance to payers.
See for yourself how helpful a Payer Summary Report can be by clicking on the image below to download a sample report:

If you’re already using Vista for post-treatment outcomes and will be negotiating soon with one of your major payers, email us with the name of the payer and the date you need the report by. We want your negotiation to be successful, so we’ll do everything in our power to provide you with compelling data that speaks your payer’s language. There is no additional charge. 😊
If you’re not already a member of the Vista Research Network, please schedule a Discovery Call now. A year from now, when you’re deep in renewal discussions and have clear, payer-specific outcomes data in hand, you’ll be negotiating from a position of strength. And it costs far less than you think to collect outcomes data that gives you real leverage in those conversations.
Clear, payer-specific outcomes data changes the conversation. It shifts you from defending your rates to demonstrating your value. But knowing how to translate that data into real reimbursement increases is a separate skill. That’s why I’ve invited two experts who have done exactly that to share how they approach these negotiations.
FORUM - Successfully Negotiating Higher Reimbursement Rates
Contract renewals aren’t real negotiations unless you walk in prepared. Join Maks Donilin and Ryan Soave of The GrowthMD for a candid, hands-on session where they’ll pull back the curtain on the strategies and leverage points they’ve used to win higher reimbursement rates in today’s brutal negotiating environment. We’ll cover:
The metrics commercial payers actually care about
How to obtain and use competitive rate intelligence effectively
How to move beyond check-the-box conversations and into discussions with people who can actually say yes
Thursday, February 19th from 2:00 – 3:00 p.m. EST
(11:00-12:00 p.m. PST; 12:00-1:00 p.m. MST; 1:00-2:00 p.m. CST)
The session will begin with a 20–25 minute discussion where I’ll ask Maks and Ryan to share what has worked for them in securing meaningful reimbursement increases. We’ll then turn off the recording and move into a frank, off-the-record conversation where participants can ask hard questions and talk about the real challenges their teams are facing. To keep the conversation practical and intimate, attendance is limited to the first 40 registrants.
Hope to see you next week.



