As much as we wish it were otherwise, recovering from addiction takes time. The longer a patient stays in a protective treatment environment, the higher the likelihood they will be successful in overcoming their addiction.
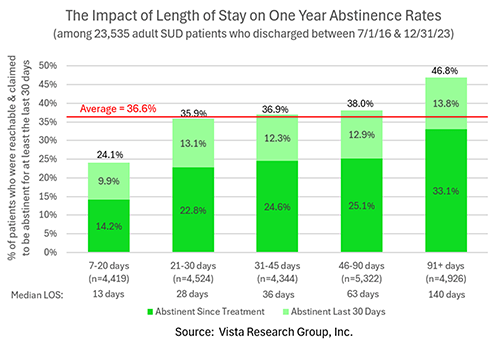
Vista’s post-treatment outcomes research among 23,535 adult SUD patients shows the dramatic impact length of treatment stay has on recovery rates:
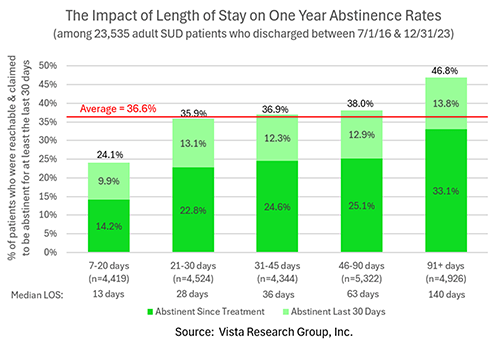
Only 24.1% of patients who were in treatment for 7 to 20 days were reachable and not using illicit drugs or alcohol one year after leaving treatment. Groups of patients with median lengths of stay between 28 and 63 days had one year recovery rates close to Vista’s average of 36.6%.
The best results by far were for patients who remained in treatment for more than 90 days. Close to half of these patients (46.8%) were reachable one year after leaving treatment and reported not having used any alcohol or non-prescribed drugs for at least the last 30 days. This is almost twice the recovery rate of patients who spent between 7 and 20 days in treatment.
This pattern is seen not only in those reporting being abstinent for at least the previous 30 days but also for those who remained abstinent the entire year after leaving treatment. Less than 15% of those in treatment for twenty days or less reported avoiding all drugs and alcohol for the full twelve months compared to 33% of those who were in treatment for greater than 90 days.
It’s important to note that these results don’t indicate that patients must remain in residential treatment for this period of time. Most of the centers in the Vista Research Network utilize a continuum of care model with patients stepping down to less-intensive levels of treatment over time.
Unfortunately, these findings fly in the face of the short treatment periods being authorized by many payers. Here are three ways you can help more of your patients recover:
Negotiate bundled-payment contracts that give you control over how long patients stay in treatment: After years of empty promises, value-based care has finally arrived. If your center has excellent success rates and the willingness to be held accountable for your outcomes, you should apply to join Carrum Health’s SUD Center of Excellence Network. You’ll be asked to define a standard episode of treatment along with its bundled cash price. Employers who are part of Carrum’s network will waive all co-pays and transportation costs for employees who attend your program.
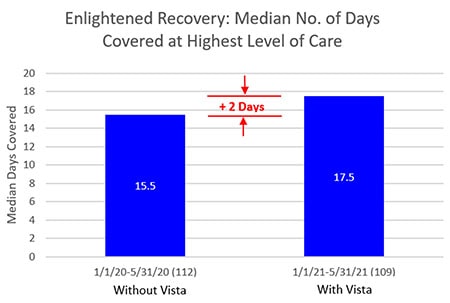
Use patient data to get more days approved: Vista’s clients have found that providing their UR team with the detailed information Vista collects from patients at intake as well as their co-occurring disorder scores throughout treatment help them negotiate more effectively with payers. In fact, one of Vista’s clients got 13% more days approved at their highest level of care after switching to Vista:

Get family commitment to complete all levels of care: Show patients and their families this data at the start of treatment. If possible, get everyone’s upfront commitment to remaining in treatment for the maximum number of days. Doing so will increase the likelihood that this will be the last episode of treatment their loved one will ever need.